Although General Hospitals, Regional and National Referral Hospitals have continued to make major contributions to essential clinical care in Uganda, numerous reports (including those of the MoH) are awash with the stark reality of lack of drugs, absence of the often inadequate health workers, delays in accessing health care services even at referral hospitals, and neglect of patients who manage to access the health care facilities, resulting into avoidable deaths among other problems.
This guide provides practical steps to reduce drowning – one of the world’s most preventable, neglected and pressing public health issues. Through 10 evidence-based interventions and strategies it is designed to help drowning-prevention practitioners – from nongovernmental organizations (NGOs) and researchers to government officials and policy-makers – approach drowning prevention in a strategic, evidence based and multi-sectoral way. It also highlights ways to harness public awareness and engagement to strengthen drowning prevention interventions.
This report presents a wide-ranging assessment and detailed findings to show by how much and in what ways improving the environment can promote health and well-being. The realization of just how much disease and ill health can be prevented by focusing on environmental risk factors should add impetus to global efforts to encourage preventive health measures through all available policies, strategies, interventions, technologies and knowledge.
Armed with the evidence of what is achievable – and needed – health-care policy-makers and practitioners alike should be encouraged in their efforts to promote healthy environments. Our evolving knowledge about environment-health interactions will support the design of more effective preventive public health strategies and interventions, directed at eliminating health hazards and reducing corresponding risks to health.
The present document was prepared in response to decision EB140(4) and is based on inputs received from WHO country offices, the regional offices for Africa, the Eastern Mediterranean and South-East Asia, together with relevant departments at headquarters. Common templates and structured interviews were provided to solicit inputs for the report, an initial draft of which was presented to a meeting of Member States on 28 April 2017.
This report limits itself to a short summary section in respect of human resource risks and associated mitigation efforts, since these issues are already included in the Annex to document A70/14. That Annex should be read in conjunction with this report to obtain a holistic understanding of the human resources, programmatic and financial risks arising from polio transition, and in order to inform the debate under the agenda subitem on polio transition planning, for which this report has been prepared.
With more than 56% of the population below 18 years of age, and over 78% under the age of 35, Uganda’s vision of becoming a middle-income country by 2040 remains highly contingent on the Government’s ability to safeguard its children’s right to contribute to national development.
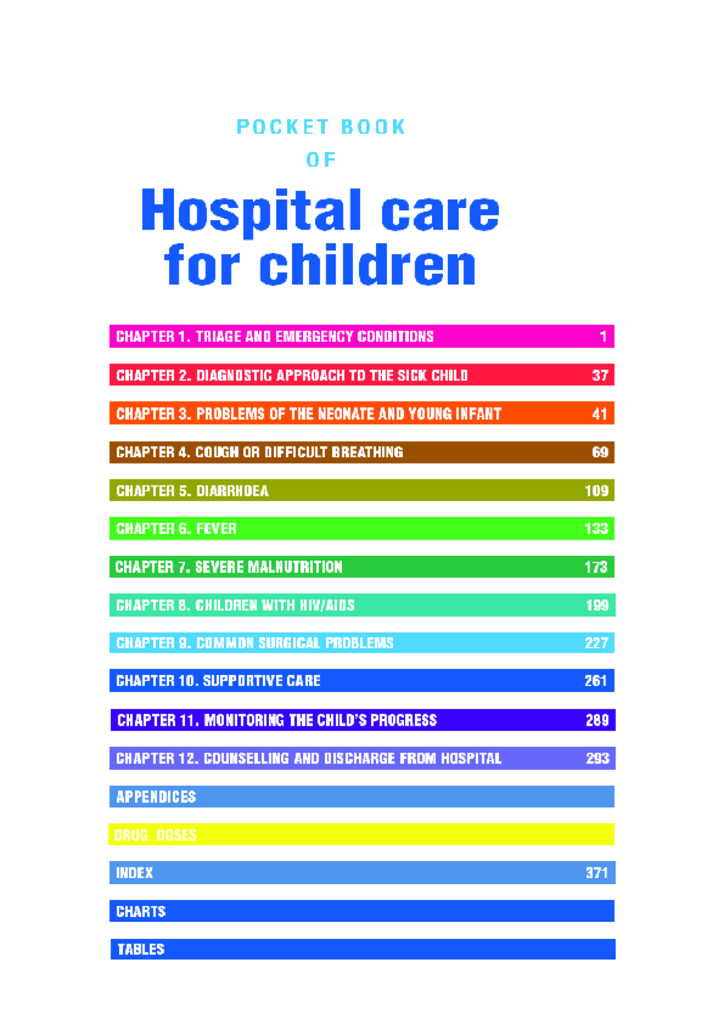
The Pocket book is part of a series of tools for improving the quality of care for severely ill children and is consistent with the Integrated Management of Childhood Illness (IMCI) guidelines for outpatient management of sick children. It is for use by doctors, senior nurses and other senior health workers who are responsible for the care of young children at the first referral level in developing countries.
Uganda adopted the Village Health Teams (VHTs) strategy in 2001 as a bridge in health service delivery between community and health facilities. This assessment sought to establish the VHT programme functionality in Uganda.
This pocket book is for use by doctors, senior nurses and other senior health workers who are responsible for the care of young children at the first referral level in developing countries. It presents up-to-date clinical guidelines which are based on a review of the available published evidence by subject experts, for both inpatient and outpatient care in small hospitals where basic laboratory facilities and essential drugs and inexpensive medicines are available. In some settings, these guidelines can be used in the larger health centres where a small number of sick children can be admitted for inpatient care.
This document is to provide guidance for the utilization of the Primary Health Care (PHC) grants and other decentralized health grants in FY 2016/17. These guidelines should be used to prepare and implement annual work plans for both Public and Private-Not-For-Profit (PNFP) facilities as well as Private Health Provider facilities where feasible / desirable.
Anemia is a major public health problem worldwide. It affects mainly preschool children and pregnant women in low-income countries. At the global level, anemia prevalence is over 30%. In sub-Saharan Africa, anemia prevalence levels are not well documented due to inadequate and insufficient techniques used to estimate anemia in the population. However, according to the World Health Organization (WHO), anemia prevalence among pregnant women in sub-Saharan Africa is estimated at 50%. Most of the anemia is associated with an imbalance between iron intake, utilization and loss that leads to iron deficiency. Malaria, hookworm infestation, deficiency in other nutrients such as vitamin A, folic acid, and B12, and, to some extent, HIV/AIDS, are also important co-factors in sub-Saharan Africa.
The policy provides a simple set of guidelines to enable local level health care managers and providers to make the best decisions they can on what oral health strategies to implement. It is a flexible decision-making framework that enables health managers to adapt the most effective oral health interventions to the specific needs, infrastructure and resources available to each community
Oral Health is central to our daily life and well-being and experts a fundamental influence on the quality of life of every citizen of uganda.