This document offers snapshots of the Madagascar GSF experience in CLTS to a wider audience. Madagascar had all usual national level challenges that generally block or slow down the pace of scaling up of CLTS. How these challenges have been addressed and transformed into an apparently snowballing strategy has been thematically presented here.
Section A provides an overview of progress against the parameters specified in the MDG target for water and sanitation, in both urban and rural areas. It presents data for the world as a whole, and compares progress across regions. The report goes on to examine trends over the MDG period by region and by level of service. It pays particular attention to the numbers of people who have gained the highest level of service in drinking water supply – piped water on premises – and those with no service at all, who use water for drinking and practise open defecation.
The 2007 Uganda Service Provision Assessment (USPA) survey collected data from a representative sample of 491 health facilities throughout Uganda. The survey covered all levels of facilities, from HC-IIs to hospitals, and sampled facilities operated by different managing authorities, including government, private-for-profit, parastatal, and faith-based organisations.
Survey personnel collected information using facility audit questionnaires, interviews with health service providers, observations of client-provider consultations, and exit interviews with clients, not only to assess the capacity of facilities to provide quality services, but also to assess the existence of functioning systems to support these services.
The WHO/UNICEF Joint Monitoring Programme for Water Supply, Sanitation and Hygiene (JMP) has produced regular estimates of global progress on drinking water, sanitation and hygiene (WASH) since 1990. It has established an extensive global database and has been instrumental in developing global norms to benchmark progress. The JMP was responsible for monitoring the 2015 Millennium Development Goal (MDG) target 7c5 and is now responsible for tracking progress towards the 2030 Sustainable Development Goal (SDG) targets related to drinking water, sanitation and hygiene (WASH). This 2017 update is the most comprehensive assessment to date and establishes the first global baseline estimates for SDG targets 6.1 and 6.2.
The SARA-hospital/HC IV census survey was a collaborative effort between the Ministry of Health, African Development Bank, and the World Health Organization.
It was undertaken to provide information on availability of services and ability of hospitals and level IV primary care facilities to provide services to the desired national standards. The aim was to visit all the 152 hospitals and 193 level IV primary care facilities in Uganda
The purpose of this basic level training resource is to assist with the training of primary ear and hearing workers in developing countries, especially focused on Village Health Care Workers. The role of the village health care worker is vitally important for the prevention of ear and hearing disorders. An important role for the trained village health care worker is to help the patient, family and community to understand common ear diseases and hearing loss.Through this training resource, the village health care worker will be taught when to refer the patient for treatment and support. This resource covers basic methods for prevention and recognition of common ear disease and hearing loss. It also shows that, with understanding and the necessary support, people with hearing loss can play productive roles in the household, school or in the work place.
The National Healthcare Waste Management Plan identifies several opportunities and activities to advance HCWM in Uganda.
Undernutrition increases the risk of tuberculosis (TB) and in turn TB can lead to malnutrition. Undernutrition is therefore highly prevalent among people with TB. It has been demonstrated that undernutrition is a risk factor for progression from TB infection to active TB disease and that undernutrition at the time of diagnosis of active TB is a predictor of increased risk of death and TB relapse.
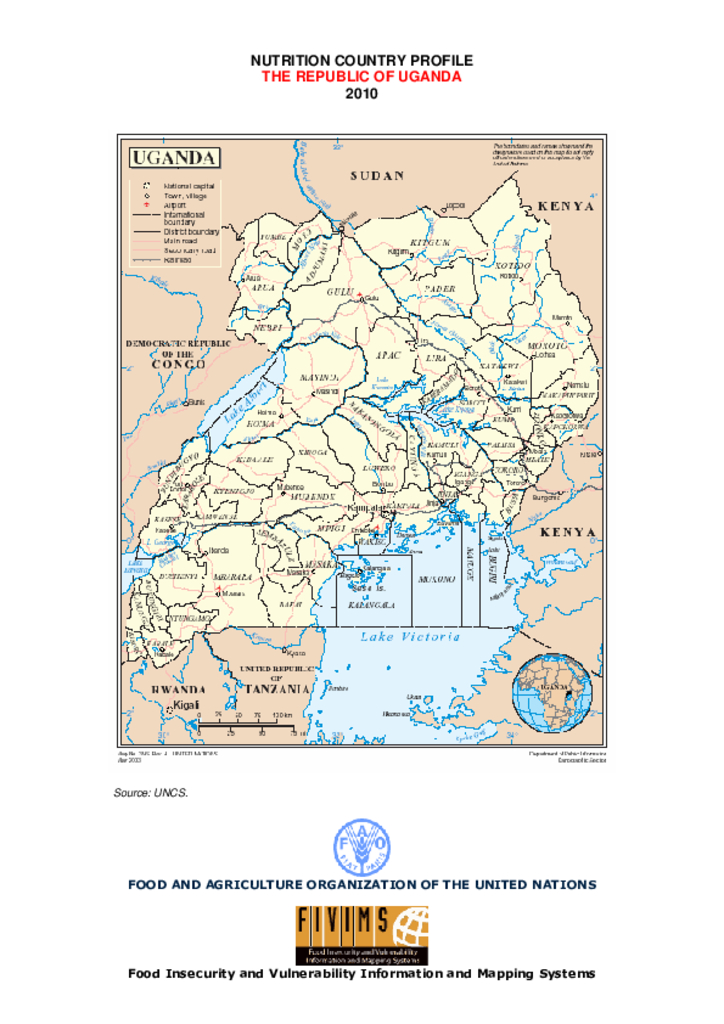
This Nutrition Country Profile of the Republic of Uganda was prepared by Dr. Joyce Kakuramatsi Kikafunda, Associate Professor of Food and Nutritional Sciences at the Department of Food Science and Technology, Faculty of Agriculture, Makerere University, Kampala, Uganda, in collaboration with Estelle Bader, Giulia Palma and Maylis Razès, Consultants, and Marie Claude Dop, Nutrition Officer, Nutrient requirements and assessment group, Nutrition and Consumer Protection Division, Food and Agriculture Organization of the United Nations.
Surgical Care at the District Hospital provides a comprehensive guide to surgical procedures that are commonly performed at the district hospital. It is intentionally limited to emergency and very common problems and is not designed as a major textbook of surgery. The manual is presented in seven parts with an initial section on organizing the district surgical service followed by clinical sections which include basic surgical procedures, the abdomen, emergency obstetrics, resuscitation and anaesthesia, acute trauma management, and orthopedics. It concludes with a course manual for teaching primary trauma care
Globally, 360 million people (about 5% of the world’s population) live with disabling hearing loss, of whom 32 million are children. The prevalence of hearing loss increases from 1.7% among children to 7% in adults (including 183 million males and 145 million females).1 Nearly 180 million people aged 65 years or older (that is, more than 30% of the population in this age group) have hearing loss that interferes with understanding normal conversational speech.2 High-quality, national and local epidemiological data on hearing loss, however, are generally lacking and this scarcity contributes to low awareness of the problem.3