The Ministry of Health recognizes that access to safe water, sanitation and hygiene (WASH) in health facilities is critical in the reduction of diseases, improved occupational health, more efficient health care services, improved staff morale and performance. The micro planning data generated will guide line ministries, local government authorities and development partners to position WASH in the health care facilities agenda within the Water and Health sectors. Additionally, it will support the development of a roadmap for achieving WASH-related sustainable development goals for health institutions.
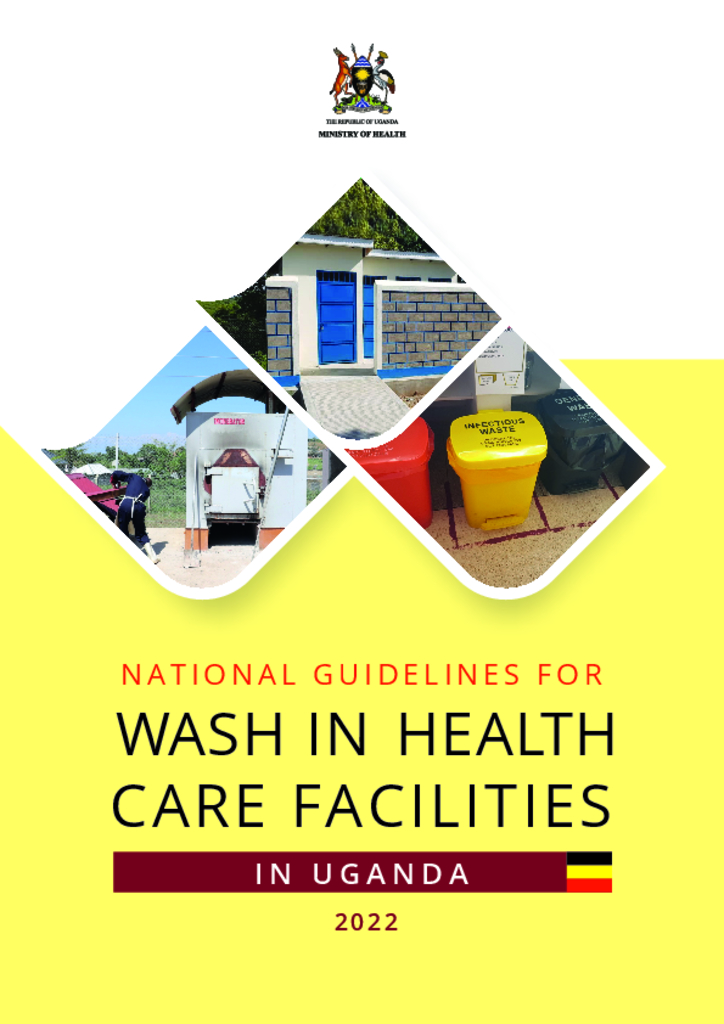
The Sustainable Development Goals (SDG) 3 and SDG 6 reinforce the need to ensure adequate WASH services, which will result in a reduction in maternal mortality, ending preventable newborn deaths, and providing quality universal health coverage. The rationale of the WASH guidelines is to document procedures and provide a framework for strategic planning, implementation of functional and effective WASH services in healthcare facilities in Uganda. These guidelines offer a basis for creating the minimum conditions required for providing healthcare services in a healthy environment for healthcare workers, patients and visitors to the healthcare premises. They also serve as a tool for monitoring the performance of WASH in health care facilities.
As countries discontinue COVID-19-specific reporting and integrate respiratory disease surveillance, WHO will use all available sources to continue monitoring the COVID-19 epidemiological situation, especially data on impact. COVID-19 remains a major threat and WHO urges Member States to maintain, not dismantle, their established COVID-19 infrastructure. It is crucial to sustain early warning, surveillance and reporting, variant tracking, early clinical care provision, administration of vaccine boosters to high-risk groups, improvements in ventilation, and regular communication.
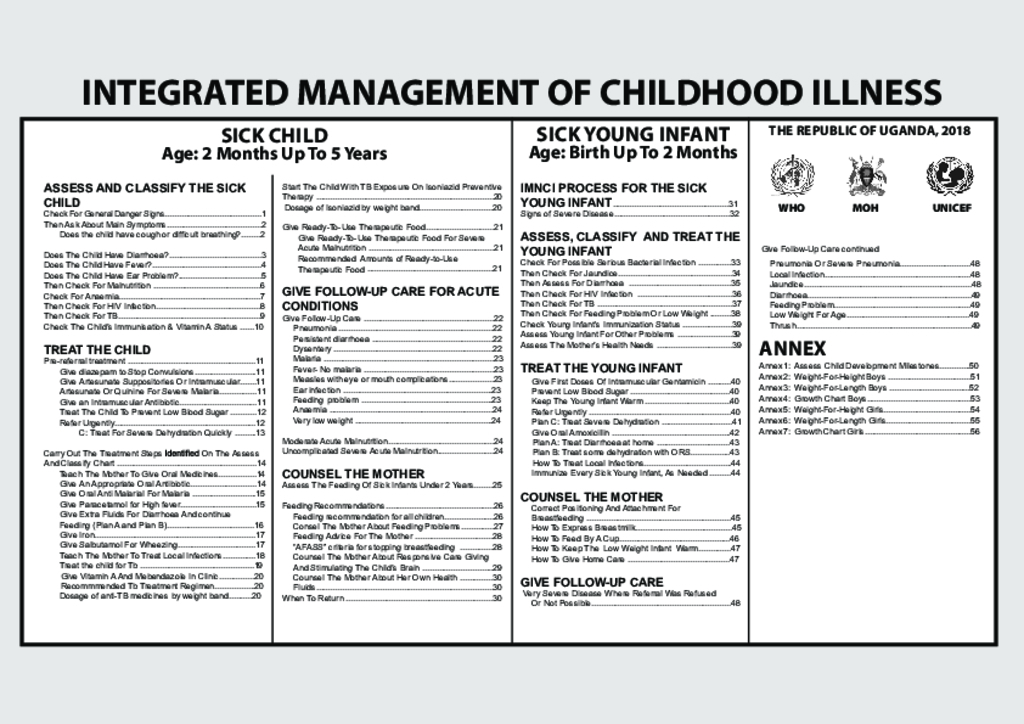
Integrated Management of Childhood Illness
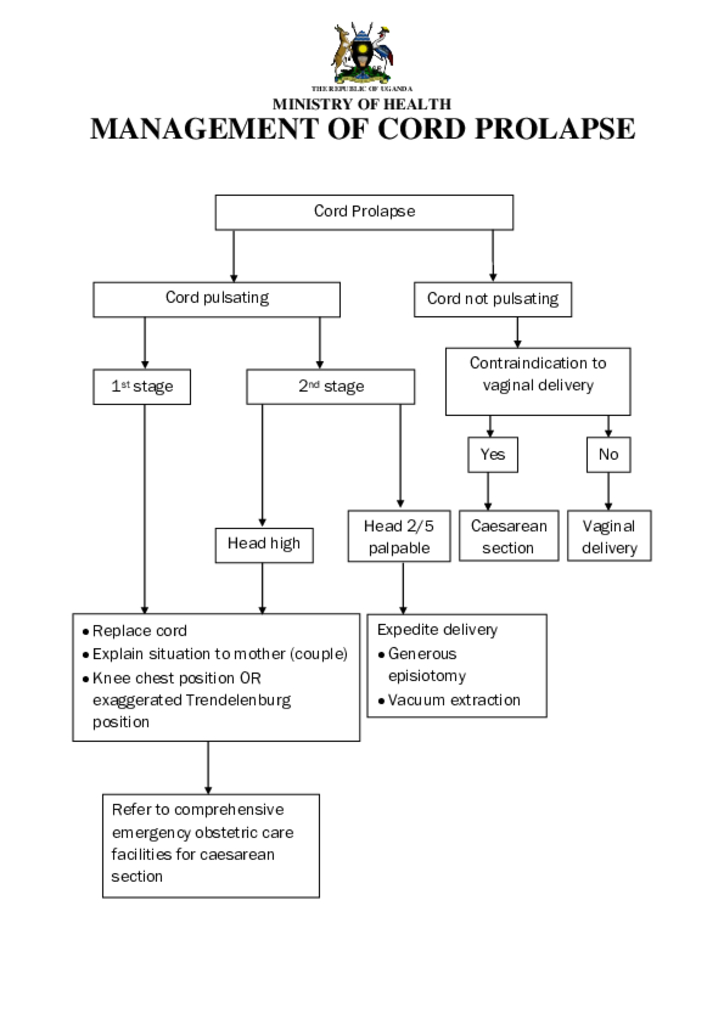
Management of Cord Prolapse
Globally, at least 1 in 3 children is not growing well due to malnutrition in its more visible forms: stunting, wasting and overweight. At least 1 in 2 suffers from hidden hunger due to deficiencies – often not visible – in essential nutrients
Tremendous progress in child survival has been made over the past two decades. The total number of deaths among children and young adolescents under 15 years of age dropped by 56 per cent from 14.2 (14.0, 14.5)1 million in 1990 to 6.2 (6.0, 6.7) million in 2018. Still, one child or young adolescent died every five seconds in 2018.
Child injuries have been neglected for many years, and are largely absent from child survival initiatives presently on the global agenda. Th rough this World report on child injury prevention, the World Health Organization, the United Nations Children’s Fund and many partners have set out to elevate child injury to a priority for the global public health and development communities. Th e knowledge and experience of nearly two hundred experts from all continents and various sectors were invaluable in grounding the report in the realities faced in many countries.
Using weight-for-height: WHO and UNICEF recommend the use of a cut-off for weight-forheight of below -3 standard deviations (SD) of the WHO standards to identify infants and children as having SAM. The commonly used cut-off is the same cut-off for both the new 2006 WHO child growth standards (WHO standards) as with the earlier National Center for Health Statistics (NCHS reference). The reasons for the choice of this cut-off are as follows
In 1993, the World Health Organization (WHO) undertook a comprehensive review of the uses and interpretation of anthropometric references. The review concluded that the National Center for Health Statistics (NCHS)/WHO growth reference, which had been recommended for international use since the late 1970s, did not adequately represent early childhood growth and that new growth curves were necessary. The World Health Assembly endorsed this recommendation in 1994. In response, the WHO Multicentre Growth Reference Study (MGRS) was implemented between 1997 and 2003 to develop international growth standards for children below 5 years of age
Although Uganda has reported a reduction in the mortality rates of children under five years of age (under-five)—from 175 deaths per 1,000 live births in 1990 to 90 deaths per 1,000 live births in 2011—child mortality and morbidity rates remain unacceptably high.1 Pneumonia, diarrhea, and malaria continue to be leading causes of mortality and morbidity among Ugandan children under-five, contributing to 40% of deaths in this age group.2 According to the Uganda national iCCM guidelines, each year, 33 million cases of malaria, diarrhea, and pneumonia go untreated. Only half (47%) of the children with symptoms of acute respiratory infection receive antibiotics,3 and only 35% of children with diarrhea receive oral rehydration salts (ORS).
Child mortality is a core indicator for child health and well-being. In 2000, world leaders agreed on the Millennium Development Goals (MDGs) and called for reducing the under-five mortality rate by two thirds between 1990 and 2015 – known as the MDG 4 target.